Food Safety Ordinance
Microbiological safety of food are stipulated in the Public Health and Municipal Services Ordinance (PHMSO) Chapter 132 section 54 that it is an offence to sell food that is unfit for human consumption.
General protection for purchases of food is also provided in Section 52 of the Ordinance when the food is not of the nature, substance, quality of the food demanded by the purchaser.
Test Analysis

Microbiological analysis is one of useful ways to assess the safety of food involved. Foodscan Analytics laboratory is able to conduct both of the conventional test method and rapid testing to fit for customer need. We are equipped with state-of-art instruments provided by the leading manufacturers. Our microbiological testing methods by traditional cultures with biochemical methods and advanced nucleic acid testing enable us to detect micro-organisms and pathogens accurately.
We offer complete testing capabilities for the detection of pathogens, toxins and indicator organisms which may be responsible for food safety and quality issues.
Food Micro-organisms and their significance
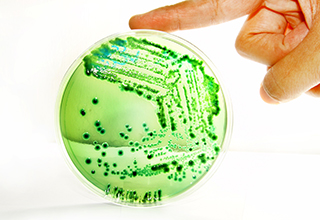
Bacteria are not visible to the naked eye. They exist in and on the human body, soil and the air, but a few types can grow in food and cause food poisoning.
With some bacteria, toxins are produced which are not destroyed by cooking – a food does not have to look, smell or taste "off " to be potentially hazardous to health.
Test Scope
Total bacterial count is the most common indicator used to reflect the quality of food product. It reflects the conditions in which the food was produced, stored or abused. At different stage of testing during production, packaging and storage, it is important for hygiene monitoring and for prediction of shelf life. There are various standard methods and recognized protocols to determine total bacterial count. Foodscan Analytics has the capabilities of performing various ranges of methodologies from conventional plate count method, multiple tube method to newly validated methods by automation.
The Total Aerobic Plate Count (APC) is one of common method to evaluation the bacterial loading. The number of bacteria in a sample that can grow and form countable colonies on Standard Methods Agar after being held at certain temperature and time.
There are various standard methods and protocols from different international recognized organisations to be adopted for APC. Foodscan Analytics has the capabilities of performing from conventional plate count method, multiple tube method to newly validated methods by automation.
This test should be requested when the normal flora of the sample in question thrive under anaerobic (oxygen void) conditions. The Count is useful to determine the overall anaerobic bacteria population of a sample.
Coliforms are a group of closely related species of organisms. These bacteria live in soil and water as well as the gut of animals. Coliforms count is generally used to as an indicator of unsanitary condition or poor hygiene practices in food production and water supply system.

E. coli is a faecal coliform which exists in the intestine of animals and men. E.coli is always used as a faecal contamination indicator to reflect poor hygienic practice in food production. Although most strains of E. coli are not regarded as pathogens, they can be opportunistic pathogens that cause infections in immunocompromised hosts. E.coli is a commonly used as an indicator of fecal contamination in food processing.
This test is an enumeration of the total Yeast and Mold population of a sample. No identifications are made, however the resultant data can be applied to internal acceptance criteria for a product or process.
Both yeasts and moulds cause various degrees of deterioration and decomposition of foods. Food products appear mould-free can be found to be contaminated upon mycological examination. Contaminated food may be slightly blemished, severely blemished, or completely decomposed, with the actual growth manifested by rot odor.
They can invade and grow on virtually any type of food at any time; they invade crops such as grains, nuts, beans, and fruits in field before harvesting and during storage. They also grow on processed foods and food mixtures. Their detectability in or on foods depends on food type, organisms involved, and degree of invasion; contamination of food by yeasts and moulds can result in substantial economic losses to producer, processor, and consumer.
E. coli 0157:H7 is one of the most pathogenic strains of E. coli. Undercooked or raw hamburger (ground beef) has been implicated in many of the documented outbreaks, however E. coli 0157:H7 outbreaks have originated from contaminated bean sprouts, unpasteurized fruit juices, dry-cured salami, lettuce, game meat, and cheese curds.
There is a widespread occurrence of Salmonella in animals, especially in poultry and swine. This organism accounts for over 50% of all reported cases of food poisoning. Environmental sources of the organism include water, soil, insects, factory surfaces, kitchen surfaces, animal feces, raw meats, raw poultry and raw seafood.
Raw meats, poultry, eggs, milk and dairy products, fish, shrimp, frog legs, yeast, coconut, sauces and salad dressings, cake mixes, cream filled desserts and toppings, dried gelatin, peanut butter, cocoa, and chocolate are foods that have been associated with Salmonella outbreaks. Symptoms usually develop between 12 - 36 hours after ingestion, causing abdominal pain, diarrhea, fever and vomiting which can last for 6 days or more.
This organism is commonly found on skin, hair and mucous membrances, and very high concentrations are often found in wounds, sores or septic spots. They can readily be transferred to food by poor handling. Foods that are frequently incriminated in staphylococcal food poisoning include meat and meat products; poultry and egg products; salads such as egg, tuna, chicken, potato, and macaroni; baery products such as cream filled pastries, cream pies, sandwich fillings, milk and dairy products. Foods that require considerable handling during preparation and that are kept at slightly elevated temperatures after preparation are frequently involved in staphylococcal food poisoning.
Staphylococci exist in air, dust, sewage, water, milk, and food or food equipment, environmental surfaces, humans, and animals. Humans and animals are the primary reservoirs. Although food handlers are usually the main source of food contamination in food poisoning outbreaks, equipment and environmental surfaces can be sources of contamination with S. aureus. Human intoxication is caused by ingesting enterotoxins produced in food by some strains of S. aureus, usually because the food has not been kept hot enough (60°C or above) or cold enough (8°C or below). Therefore, this is a good test to indicate temperature abuse of selected food products. Incubation time is short so violent vomiting and diarrhea can occur within 2 to 6 hours.
This organism is ever present in nature and can be found as a normal component of decaying vegetation, the intestinal tract of humans and other vertebrates, insects and soil.
C. perfringens is the third most common cause of food poisoning, though it can sometimes be ingested and cause no harm.
This organism is widespread in the environment. It has been involved in cases of food poisoning from ingestion of affected milk, vegetables, meats, soft cheeses, ice-cream and seafood. Listeria monocytogenes is the most significant species and can grow at refrigerator temperatures. For high risk populations (the very old, the very young, pregnant and immunocompromised) a very little amount of Listeria in food can be highly dangerous.
Bacillus cereus has ubiquitous distribution in the environment and can be isolated from a variety of processed and raw foods. However, its presence in foods is not a significant health threat unless it is able to grow. Consumption of food containing more than 105 viable cells/g has resulted in outbreaks of food borne illness. Foods frequently incriminated include: boiled and fried rice, cooked pasta, cooked meats, cooked vegetables, soups, salads, puddings and vegetable sprouts.
V. cholera is generally tramsmitted via contaminated water, ice, fruit, vegetable refreshed with sewage polluted water, raw or undercooked seafood. This bacterium may be present in human faeces, untreated sewage and marine environment.
Cholera disease occurs when V. cholera colonizes the small intestine and releases cholera toxin. Symptoms include: vomiting, watery diarrhoea, dehydration, muscular cramp and abdominal pain.

Vibrio parahaemolyticus is a bacterium in the same family as those that cause cholera. It lives in brackish saltwater and causes gastrointestinal illness in humans. It is a salt-requiring organism. When ingested, V. parahaemolyticus causes watery diarrhoea often with abdominal cramping, nausea, vomiting, fever and chills. Illness usually lasts 3 days, severe disease is rare and occurs more commonly in persons with weakened immune systems. Most people become infected by eating raw or undercooked shellfish, particularly oysters. Less commonly, this organism can cause an infection in skin when an open wound is exposed to warm seawater.





